[ad_1]
Crown
We may receive an affiliate commission from anything you buy from this article.
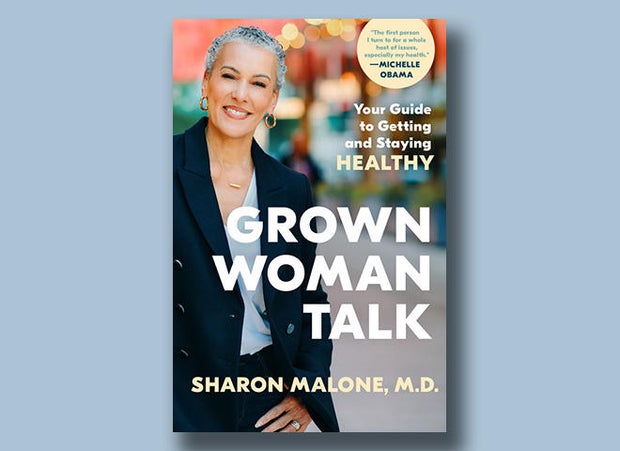
In her new book, “Grown Woman Talk: Your Guide to Getting and Staying Healthy” (published April 9 by Crown), Dr. Sharon Malone, an OB/GYN and certified menopause practitioner, addresses issues facing women who may feel marginalized about their health questions as they get older.
Among the important topics covered is perimenopause/menopause, a stage in life that has long been stigmatized but which, Dr. Malone says, has an upside.
Read an excerpt below, and don’t miss Tracy Smith’s interview with Sharon Malone on “CBS News Sunday Morning” April 7!
“Grown Woman Talk” by Sharon Malone, M.D.
Prefer to listen? Audible has a 30-day free trial available right now.
Menopause and Beyond
So, it’s been twelve months since your last period. You are now one of the estimated 2 million women in the United States who enter menopause each year. Congratulations! You’ve officially crossed over.
The average age for becoming menopausal in the United States is about 51. But who’s average? About 5 percent of women experience what is considered an early menopause, defined as having had your last period between the ages of 40 and 45. Whether early menopause occurs naturally or because of surgery, medication, or certain medical conditions, it puts you at higher risk for the long-term consequences of menopause. Fortunately, only about 1 percent of women go through menopause before the age of 40. But the symptoms that we associate with perimenopause/menopause can show up as early as ten years before the final menstrual period. This means that about 6 percent of women can become symptomatic and experience suboptimal fertility in their 30s! Thus, knowing the signs and symptoms as well as your family history are extremely important in not only making an accurate diagnosis, but in effective family planning.
There are currently over 55 million menopausal women in the United States alone. The latest CDC provisional life expectancy statistics (2021) report that the life expectancy for white women is 79.2 years; for Black women, that figure is 74.8; for Hispanic women, it is 81; and the ethnic groups with the highest and the lowest life expectancies are Asians at 85.6 and Native American/Alaskans at 69.2. Of note, all of these numbers have decreased by almost two years since COVID. Let’s hope and pray that these numbers will soon return to pre-pandemic levels. Whether they do or not, most women in this country will spend on average twenty-five to thirty years in menopause. Think about that: You are likely to spend as much time in menopause as you have spent in any other reproductive phase of your life. So, why do we talk so little about it? … At this point, inquiring minds want to know, what now?
This may not be your favorite answer, but as with most things in life, it depends. For starters, what are your menopausal symptoms? And how severe are they? Although your hot flashes, mood swings, and brain fog will likely get better after your hormones settle down, some of those other thirty-four symptoms will not. (Think dry skin, dry vagina, thinning hair, and low libido, to name a few.) And for a few unfortunate souls, intense hot flashes can persist for years, even decades.
Any of these symptoms can and should be treated if they are diminishing your quality of life. But the bigger health issues, the ones that can exact a heavy toll for many years after menopause, these are the ones I want you to pay special attention to. I’m talking about cardiovascular disease, osteoporosis, and Alzheimer’s disease, which can snake their way in, uninvited and under the radar.
Now that I’ve got your attention, you should also know that 80 percent of women will also experience the genitourinary syndrome of menopause (GSM), which is a constellation of symptoms, such as vulvar and vaginal dryness, painful sex, and urinary problems that tend to worsen if they’re not addressed. So, don’t sit idly by “dealing with it.” This is no surrender-Dorothy, woe-is-me situation.
Now more than ever, women are speaking out about menopause openly and honestly, and are demanding answers. We are setting new standards for what aging gracefully and healthily looks like. Michelle Obama, Tracee Ellis Ross, Maria Shriver, and Oprah Winfrey have shared their menopause stories, changing the face of what health and strength look like at 50, 60, and 70. This is not your grandmother’s menopause! Nor should it be.
Understanding and taking better care and control of this time in your life matters. So, let’s be good stewards of our health as we age. That means knowing what your objectives are, what your particular risks are, and what to do about them once you’ve identified them. There is no one-size-fits-all solution, but there are options—all of which are going to require you to be your own best advocate. Start by going to your doctor to discuss how to create a plan for healthy aging and disease prevention. Doing so can be a challenge when menopausal specialists are few and far between. I firmly believe that you deserve access to quality care, whether you live in Yazoo City or New York City. But you and I have lived long enough to know that people are not always going to give us what we deserve, we’re going to have to go after it. So, no matter where you live, be unrelenting in your pursuit of the information you need to make good choices.
Dr. Sharon’s Rx for a Mah-velous Fourth Quarter
- Exercise regularly. Remember our exercise goals after 50 are different. Do not exercise because you are hoping to lose weight. You will be disappointed. Exercise after 50 is to preserve your muscle mass and strength as you age. Include resistance and core exercises to improve balance. Maintaining a strong core will decrease your risk of falling and increase your chances of being able to get yourself off the floor if you do.
- Mind your cardiovascular health. This begins with eliminating the things that increase your risk. Treat hot flashes and sleeplessness. Watch your weight. Take your medications for hypertension … every day!
- Maintain a calcium- and vitamin D-rich diet. You start to lose bone mass after menopause if you do not take estrogen. Although calcium and vitamin D do not prevent osteoporosis, they are key nutrients that are necessary for bone health, as well as many other bodily functions. Your calcium intake after 50 should increase to 1,000–1,200 mg daily with vitamin D 600–800 IU daily. Dietary sources are always better than supplements. Now I know why my mother made me take cod-liver oil in the winter. My mother was a genius! Get your vitamin D levels checked if you are lactose intolerant, are darker-skinned, use total body sunscreen, wear a hijab, or if you don’t like the outdoors. Your body can make its own vitamin D, but only if you have exposure to sunlight at least twenty minutes a day.
- Don’t smoke! Smokers have a higher incidence of osteoporosis and more severe menopausal symptoms.
- Know your bone density. I recommend getting a baseline DEXA Scan as soon as you’re menopausal, especially if you have a family history of osteoporosis, have had a fracture in the past, smoke, or have poor dietary calcium intake—e.g., are lactose intolerant—or if you are currently taking thyroid medication. The standard recommendation is 65, but don’t let that be your guide.
- Consider menopausal hormone therapy. Estrogen is FDA-approved for osteoporosis prevention and is the most effective medication for relief of menopausal symptoms.
- Use topical vaginal estrogen. It not only prevents vaginal dryness and preserves sexual function, but also decreases the risk of UTIs as you age.
From the book “Grown Woman Talk: Your Guide to Getting and Staying Healthy” by Sharon Malone, M.D. Copyright © 2024 by Sharon Malone, M.D. Published in the United States by Crown, an imprint of the Crown Publishing Group, a division of Penguin Random House LLC.
Get the book here:
“Grown Woman Talk” by Sharon Malone, M.D.
Buy locally from Bookshop.org
For more info:
 Latest Breaking News Online News Portal
Latest Breaking News Online News Portal